What’s the big idea?
Cancer research used to focus mainly on tumor mutations and the immune system. Now a third player keeps showing up: microbes — the bacteria (and other microorganisms) in your gut and even inside tumors themselves. Researchers are finding microbial communities can shift inflammation, train immune cells, and change how well treatments work.
Three ways microbes are reshaping cancer research
1) Microbial “fingerprints” as biomarkers
Researchers are building microbiome signatures that correlate with response, resistance, and side effects. Expect more trials that combine tumor genomics with stool (or tumor) microbiome profiling to guide therapy choices.
2) Microbiome “tuning” to boost immunotherapy
Clinical studies are testing approaches like diet shifts, targeted probiotics, and fecal microbiota transplantation (FMT) to help some non-responders respond — especially alongside checkpoint inhibitors. It’s still experimental, but it’s moving fast.
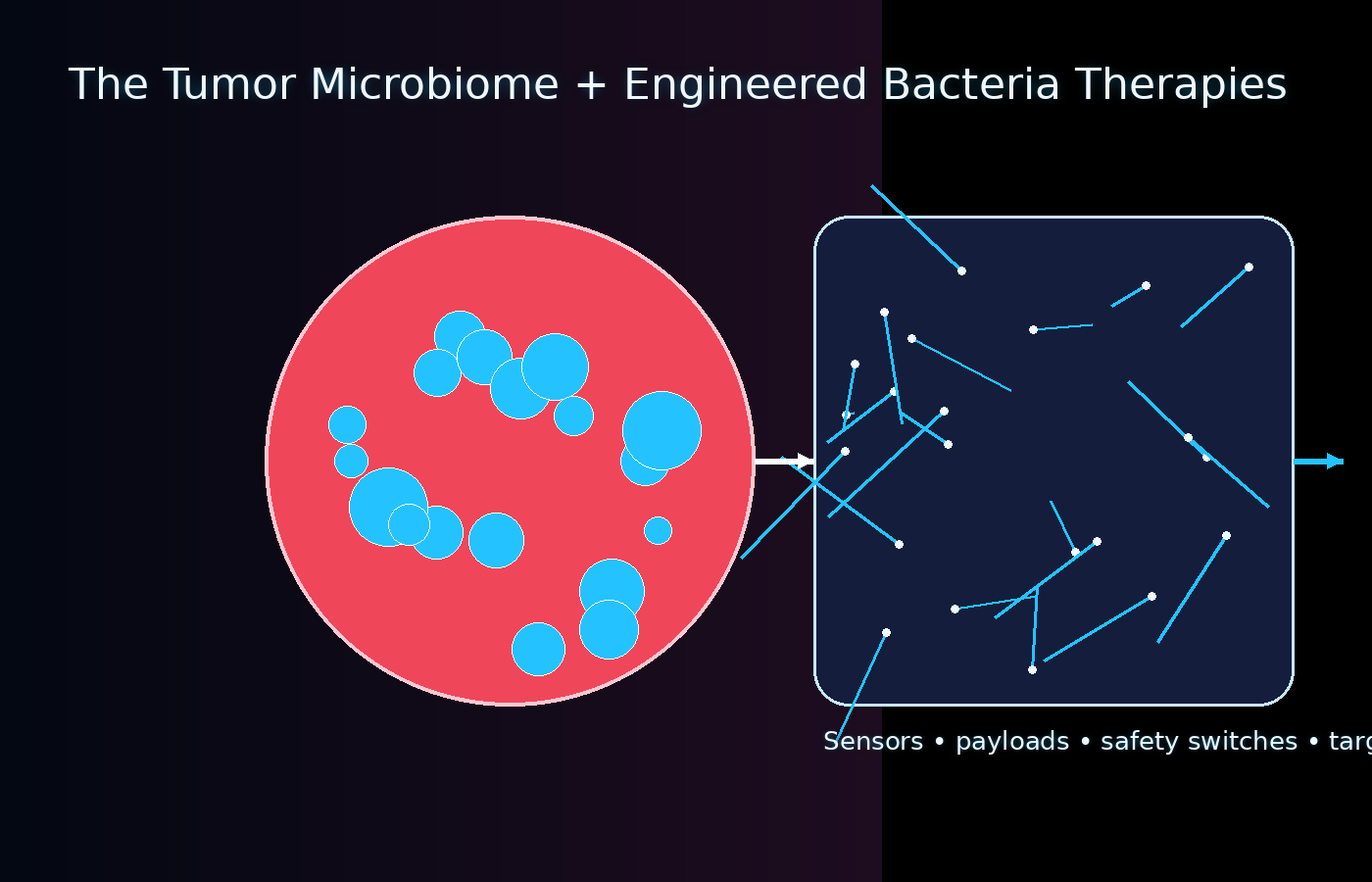
3) Engineered bacteria as “living medicines”
Some bacteria naturally thrive in low-oxygen tumor cores. That’s being turned into an advantage: engineered strains can sense tumor conditions and deliver payloads locally — with safety switches designed to limit risk.
What the next 5–10 years likely brings
- Microbiome-aware clinical trials becoming standard, especially for immunotherapy combinations.
- Safer microbiome therapeutics (capsules and defined microbial consortia) to reduce infection risk compared to broad transfers.
- Antibiotic stewardship in oncology with more awareness of when antibiotics may blunt immunotherapy response.
- Tumor microbiome mapping to understand bacteria living inside tumors and how they affect drug penetration and immune activity.
- Programmable bacterial therapies paired with immune-cell treatments for targeted tumor “re-wiring.”
Reality check
This is promising research — not a shortcut cure. Microbiomes vary wildly between people, and results don’t always translate across populations. The hard part is proving cause (not just correlation) and creating safe, repeatable interventions.
Watch: 3 videos
Immunotherapy and gut bacteria (Dana-Farber Cancer Institute)
A clinician-friendly overview of how gut bacteria can influence immune checkpoint therapy and why researchers are using microbiome data to understand response and resistance.
Promising treatment to cure advanced melanoma (FMT + immunotherapy)
Explains fecal microbiota transplantation (FMT) and how early trials test whether changing the gut microbiome can help some patients respond to immunotherapy.
Engineering bacteria for tumor-targeted therapy (Northwestern Feinberg)
Walkthrough of programmable bacteria—how microbes can be designed to sense tumor conditions, deliver payloads locally, and include safety ‘kill switches’.
Share this article
Study links
- NCI: Gut bacteria affect immunotherapy response
- NCI: Engineered E. coli can help the immune system attack tumors (2024)
- PubMed: FMT + anti-PD-1 immunotherapy in advanced melanoma (phase I)
- Science: FMT + anti–PD-1 overcame resistance in melanoma (2021)
- NIH NIBIB: Engineered bacteria prime tumors for selective elimination (2024)
- NCI CCR: Better microbes, better immunotherapy